Occipital Neuralgia: Signs, Causes, and Relief Options
If your pain starts at the base of your skull and shoots upward—or feels like stabbing, zapping, or burning—it may be nerve pain, not a typical headache.
Occipital neuralgia happens when the occipital nerves (which travel from the upper neck to the scalp) become irritated or inflamed. The pain often feels electric, sharp, or hot. It can be triggered by neck movement, posture strain, or light touch.
This guide explains:
- How to recognize nerve-based head pain
- What causes occipital neuralgia
- Differences between occipital neuralgia, migraine, and tension headaches
- What relief options exist, from lifestyle changes to medical care
What Is Occipital Neuralgia?
Occipital neuralgia is a neuropathic pain condition involving the greater or lesser occipital nerves. These nerves originate in the C2-C3 spinal roots and travel upward through neck muscles to the scalp. When irritated, they send pain signals interpreted as sharp, electric, or burning.
Common pain descriptions include:
- “Lightning bolts” in the back of the head
- Sharp, stabbing pain behind the ear
- Scalp burning or tingling
- Pain when brushing hair or lying down
- Shooting pain triggered by neck movement
Related Entities
Next, we’ll review the key symptoms to help distinguish nerve-based head pain.
Symptoms: When Head Pain Is Actually Nerve Pain
Occipital neuralgia symptoms typically include:
- Sudden, sharp pain at the skull base
- Pain that radiates to the scalp, eye, or temple
- Hypersensitive scalp (painful to touch)
- Neck tightness or coexisting neck pain
- Symptoms triggered by posture or movement
This pain often mimics migraines, but differs in quality. Migraines often pulse and involve nausea or light sensitivity. Occipital neuralgia pain is sharper, shorter, and often electric in nature.
Symptom Comparison Table
Next, we’ll explore what causes these nerve-related symptoms.
What Can Trigger Occipital Nerve Pain?
Known triggers of occipital neuralgia include:
- Neck muscle tension or spasm
- Postural stress, like working long hours at a desk
- Whiplash or cervical injury
- Chronic nerve compression
- Overactive pain signaling from central sensitization
Examples of Trigger Patterns
- Pain starting after car accident → Whiplash strain on occipital nerves
- Desk worker with poor posture → Muscle tightening around nerve pathway
- Long-standing neck pain → Sensitized nerve endings trigger scalp pain
The nervous system may stay in a hyper-reactive state, even after the original injury resolves. That’s why some patients don’t have a clear, isolated cause.
Next, we’ll compare occipital neuralgia with other common headache types.
Occipital Neuralgia vs. Migraine vs. Tension Headache
Occipital neuralgia differs in both origin and symptom pattern.
Key Differentiators:
Recognizing the pattern helps guide proper care. In the next section, we focus on relief options.
Relief Options: What Can Help Occipital Neuralgia?
1) Calm Nerve Sensitization
Neuropathic pain involves a hyperactive pain pathway. To reduce irritation:
- Maintain consistent sleep routines
- Reduce stress via breathing or relaxation exercises
- Avoid sustained neck postures (use posture breaks)
2) Address Mechanical Neck Factors
The neck’s mobility and muscle tone can impact nerve pressure.
- Physical therapy may reduce muscle tightness
- Targeted stretches improve cervical alignment
- Ergonomic adjustments reduce daily strain
3) Consider Non-Invasive, Drug-Free Relief
Scrambler Therapy is an FDA-cleared treatment for chronic nerve pain. It delivers non-pain signals to the brain to “override” persistent pain input.
Benefits of Scrambler Therapy:
- Non-invasive and drug-free
- Suitable for chronic, nerve-based pain
- May reduce reliance on medications
4) Seek Medical Evaluation if Needed
Medical care may involve:
- Nerve blocks to calm inflammation
- Medications (neuropathic pain agents like gabapentin)
- Imaging if other causes need exclusion
📌 Get evaluated if pain is:
- Severe and new
- Associated with numbness, weakness, or coordination loss
- Accompanied by other neurological signs
Next, we’ll describe typical patient patterns seen in the clinic.
What We See in Clinic
Many patients report being misdiagnosed with regular headaches when the pain feels nothing like it. Common phrases include:
- “It feels like zaps in my skull”
- “My scalp hurts when I touch it”
- “It starts at my neck and shoots up”
In clinic, we:
- Map the pain origin and referral pattern
- Explore history and triggers
- Build a recovery plan, including education, therapy, and relief options
Next, we outline when to seek urgent medical attention.
When to Seek Urgent Care
Go to an ER or call emergency services if you experience:
- Sudden, severe “worst-ever” headache
- Weakness, slurred speech, or visual changes
- Fever, confusion, or stiff neck
- Head pain with fainting or neurological symptoms
These may signal serious conditions that need immediate intervention.
Next, see what steps help move forward if you suspect occipital neuralgia.
Next Step if You Suspect Occipital Neuralgia
To help your clinician assess the pain, track:
- Where the pain starts
- What triggers it (movement, stress, touch)
- How it feels (sharp/electric vs pressure/dull)
- Whether sleep or posture affects symptoms
📌 Meet Dr. Markson
📌 Patient Success Stories
FAQ: Occipital Neuralgia
What causes occipital neuralgia?
Irritation or compression of the occipital nerves, often due to muscle tension, posture strain, or past neck injury, can trigger pain.
How is occipital neuralgia diagnosed?
Clinicians diagnose by reviewing symptoms, pain patterns, physical exam findings, and sometimes by using nerve blocks or imaging.
Is occipital neuralgia permanent?
Not always. With treatment, many people reduce or resolve symptoms through therapy, nerve blocks, or neuromodulation techniques.
Can stress make occipital neuralgia worse?
Yes. Stress increases muscle tension and nervous system sensitivity, both of which can intensify symptoms.
What treatment helps best for occipital neuralgia?
Treatment depends on severity. Options include physical therapy, lifestyle changes, Scrambler Therapy, nerve blocks, or medications.
Experiencing Chronic Pain in South Florida?
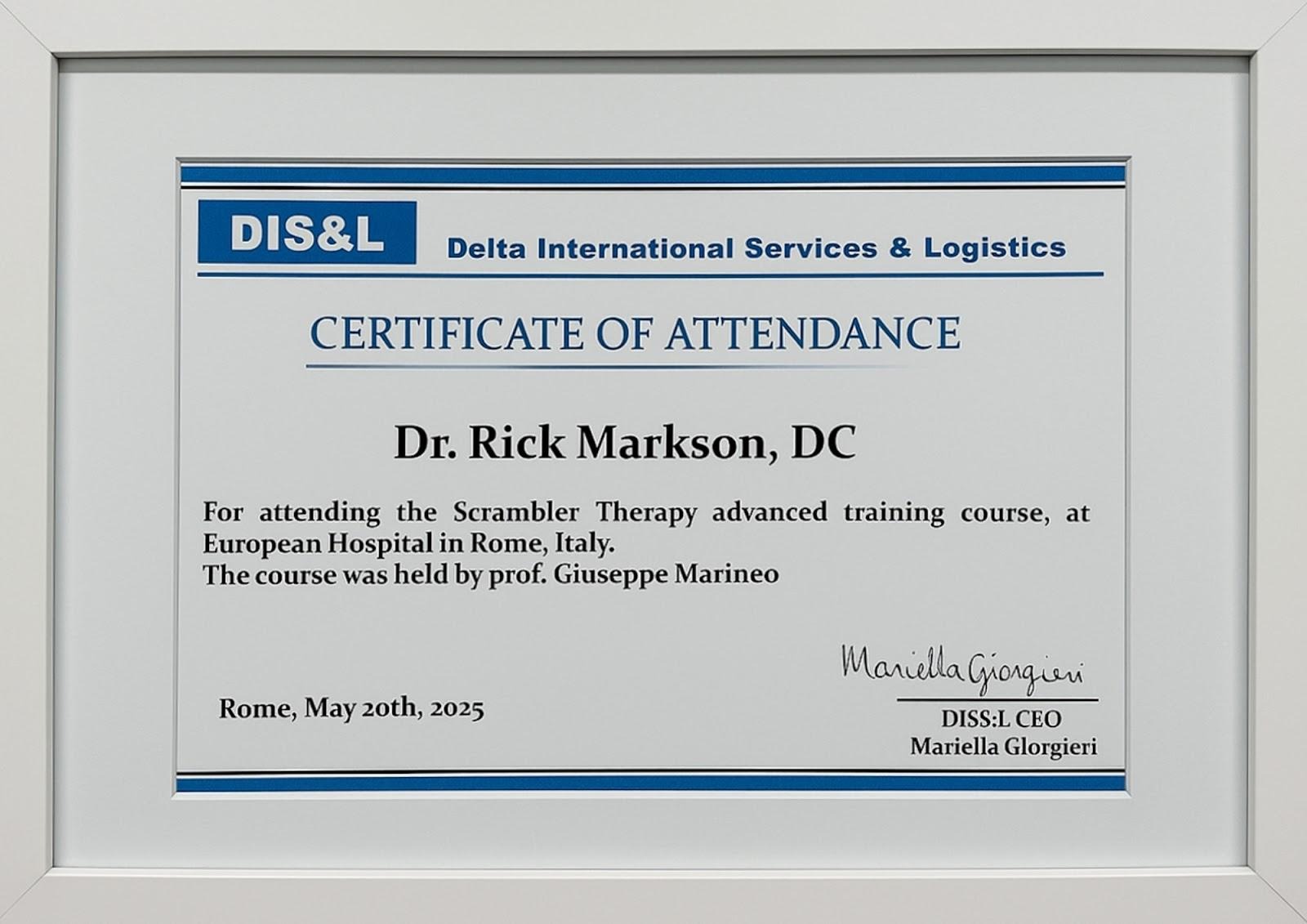
Discover South Florida Scrambler Therapy is one of the nation’s leading clinics for noninvasive chronic pain relief, offering FDA-cleared Scrambler Therapy® for adults and children. Co-founded by Dr. Rick Markson, one of the few practitioners worldwide to receive advanced certification directly from the therapy’s inventor in Rome, our clinic delivers globally recognized expertise with compassionate, personalized care. If you or a loved one is living with treatment-resistant nerve pain, we invite you to schedule a consultation and explore a life beyond pain.
Recommended links that shows legitimacy of scrambler therapy:
Scrambler Therapy FDA FDA 510(k) database
Scrambler Therapy delivers 80%–90% pain reduction for patients suffering from nerve-related pain.
Pain Physician Journal study on Scrambler Therapy’s effectiveness
Scrambler therapy is a non-invasive, opioid-sparing treatment for chronic pain.
Recommended Reads:
📘 What is scrambler therapy?
📘 What to Expect During a Scrambler Session
📘 CRPS Pain Relief Without Drugs—Real Patient Stories
📘 Conditions that scrambler therapy can treat
Take the Next Step: Free Consultation at South Florida Scrambler

Every day counts when we suffer from chronic pain. South Florida Scrambler Therapy offers a free initial consultation to determine if Scrambler is right for you. Schedule Today:
- Speak directly with Dr. Rick Markson’s team
- Learn about treatment protocols and insurance
- Complete a customized treatment plan
- Start seeing results within days, not months
📞 Call Now or Visit website: www.southfloridascramblertherapy.com
📍 We serve Palm Beach, Fort Lauderdale, and Miami from our location at 100 NW 100th Ave, Plantation
You Can Follow Us through Our Social Media:
📸Instagram—Day-in-the-life stories from our patients
👍Facebook—Success journeys and community support
You deserve to laugh, and enjoy life without pain. The journey starts here
Patient Reviews
Start Your Nerve Pain-Free Journey Today







