Pudendal Neuralgia: Pelvic Nerve Pain Options in 2026

Pelvic nerve pain often leads to delayed diagnosis and frustration. Pudendal neuralgia describes neuropathic pain caused by irritation or dysfunction of the pudendal nerve. This nerve controls sensation and some motor function in the pelvic region. The condition affects all genders and often remains underrecognized in routine care.
Understanding how the pudendal nerve functions helps explain why symptoms are persistent and why care often requires a specialized approach.
In the next section, you will read how this nerve works and why irritation causes pain.
What Is Pudendal Neuralgia?
Pudendal neuralgia is chronic pelvic pain caused by abnormal signaling from the pudendal nerve. The pudendal nerve originates from the sacral spine, travels through the pelvis, and innervates the perineum, genitals, and anal region.
When the nerve becomes compressed, overstretched, or sensitized, it sends pain signals even without tissue damage. Nerve pain differs from muscle pain. Patients often describe it as burning, sharp, electric, or deep pressure.
This mechanism explains why standard imaging often appears normal. The next section outlines the most common symptom patterns reported in clinical settings.
Common Symptoms of Pudendal Nerve Pain
Pudendal neuralgia produces sensory symptoms that follow the nerve pathway. Commonly reported symptoms include:
- Burning or aching pain in the perineum or pelvis
- Pain that increases with sitting and improves when standing or lying down
- Genital numbness, tingling, or hypersensitivity
- Rectal, vaginal, or penile discomfort
- A sensation of fullness or foreign body without visible cause
Symptoms often worsen as the day progresses. Many patients report partial relief when pressure on the pelvis is reduced. These features help distinguish pudendal neuralgia from other pelvic pain conditions, which leads into why diagnosis is challenging.
Why Pudendal Neuralgia Is Hard to Diagnose
Pudendal neuralgia lacks a single confirmatory test. MRI and CT scans frequently appear normal because nerve dysfunction does not always cause visible structural changes.
Clinicians rely on:
- Symptom location along the pudendal nerve distribution
- Pain behavior such as sitting intolerance
- Clinical history including triggers or prior pelvic events
- Response to targeted treatments such as nerve blocks
Misdiagnosis is common. Patients are sometimes told symptoms are psychosomatic or unexplained. A careful clinical evaluation is essential before treatment planning. Understanding causes helps clarify why symptoms develop.
What Causes Pudendal Neuralgia?
Prolonged Sitting or Cycling
Sustained pressure on the pelvic floor can compress the pudendal nerve. Long distance cycling and prolonged seated work are frequently reported risk factors.
Pelvic Surgery or Childbirth
Surgical procedures and vaginal deliveries can stretch or irritate the nerve. Scar tissue may alter normal nerve mobility and signaling.
Musculoskeletal Tension and Pelvic Floor Dysfunction
Chronic pelvic floor muscle tension can narrow nerve pathways. This mechanical stress increases nerve sensitivity and pain signaling.
Recognizing the cause guides treatment selection, which is discussed next.
Pudendal Neuralgia Treatment Options
Effective care usually combines multiple strategies. Single treatments rarely address all contributing factors.
Medications
Neuropathic pain medications may reduce nerve signaling. Common classes include anticonvulsants and antidepressants. Side effects limit long term use for some patients.
Pelvic Floor Physical Therapy
Specialized physical therapists address muscle tension, posture, and nerve mobility. Therapy focuses on reducing mechanical irritation rather than strengthening alone.
Pudendal Nerve Blocks
Image guided nerve blocks can provide temporary pain relief. Clinicians also use blocks diagnostically to confirm nerve involvement.
Non Invasive Neuromodulation
Non-invasive neuromodulation targets abnormal nerve signaling without injections or surgery. Scrambler Therapy uses surface electrodes to retrain pain pathways.
- Learn more about this option here: /treatments/scrambler-therapy
- Related condition overview: /conditions/neuropathic-pain
Treatment planning should reflect symptom pattern, duration, and patient tolerance.
The next section explains how this approach works in real clinical settings.
What We See in Clinic
Many patients seek care after years of dismissal or incomplete explanations. Education often becomes the first therapeutic step. Understanding that pain originates from nerve dysfunction helps reduce fear and uncertainty.
Clinical experience shows improved outcomes when care combines education, physical therapy, and nerve focused treatments rather than relying on a single modality.
The following FAQs address common questions patients ask during early consultations.
FAQs
What triggers pudendal neuralgia?
Common triggers include prolonged sitting, cycling, pelvic surgery, childbirth, and chronic pelvic floor tension.
Is pudendal neuralgia permanent?
No. Symptoms vary. Many patients experience improvement with appropriate treatment and lifestyle adjustments.
How is pudendal neuralgia diagnosed?
Diagnosis relies on clinical evaluation, symptom patterns, and response to targeted treatments rather than imaging alone.
Are there non surgical treatments for pudendal neuralgia?
Yes. Physical therapy, medications, nerve blocks, and non-invasive neuromodulation are commonly used.
Can men have pudendal neuralgia?
Yes. The condition affects people of all genders.
Medical Disclaimer
This content is for educational purposes only and does not replace medical advice. Diagnosis and treatment should be guided by a qualified healthcare professional.
Experiencing Chronic Pain in South Florida?
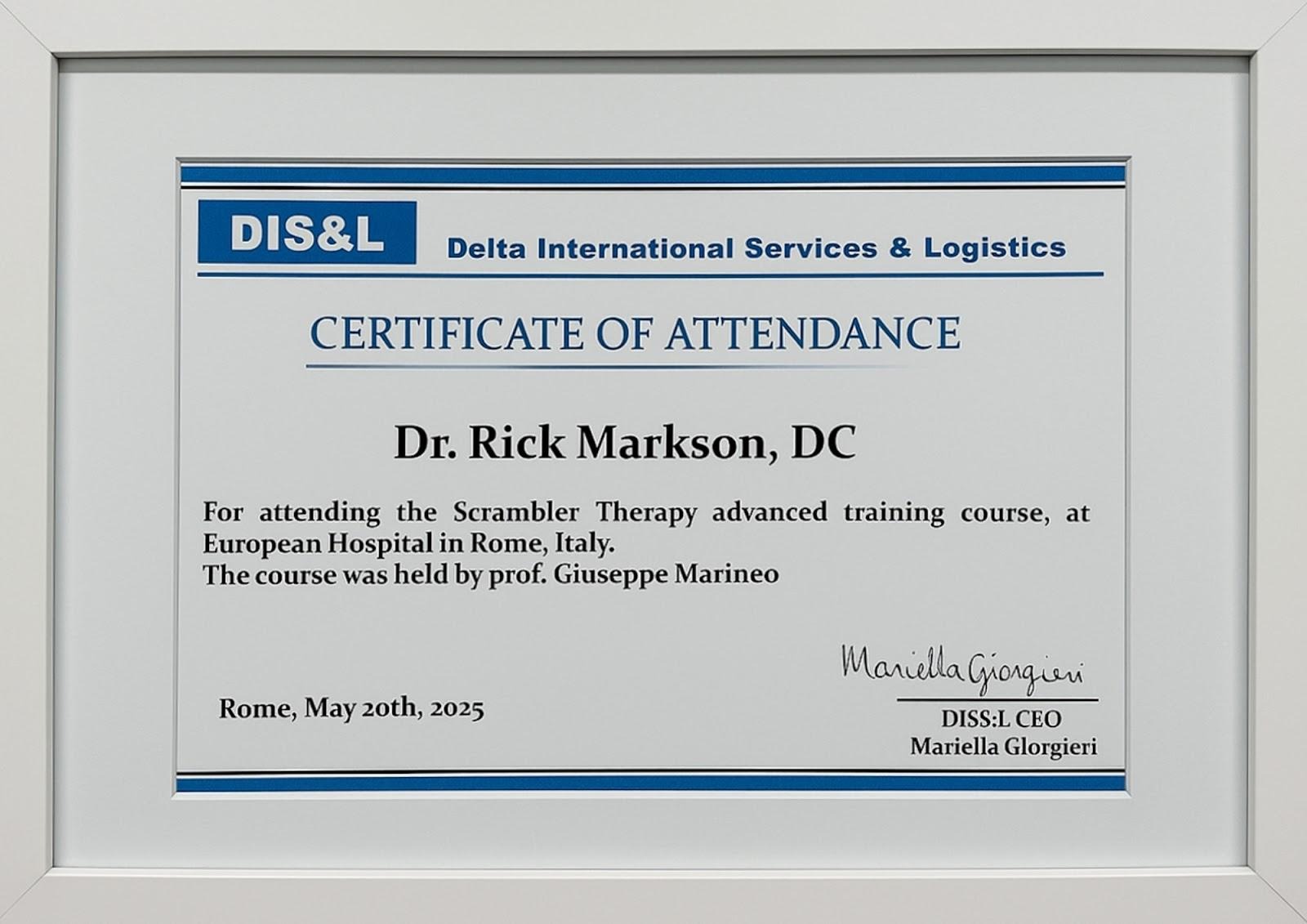
Discover South Florida Scrambler Therapy is one of the nation’s leading clinics for noninvasive chronic pain relief, offering FDA-cleared Scrambler Therapy® for adults and children. Co-founded by Dr. Rick Markson, one of the few practitioners worldwide to receive advanced certification directly from the therapy’s inventor in Rome, our clinic delivers globally recognized expertise with compassionate, personalized care. If you or a loved one is living with treatment-resistant nerve pain, we invite you to schedule a consultation and explore a life beyond pain.
Recommended links that shows legitimacy of scrambler therapy:
Scrambler Therapy FDA FDA 510(k) database
Scrambler Therapy delivers 80%–90% pain reduction for patients suffering from nerve-related pain.
Pain Physician Journal study on Scrambler Therapy’s effectiveness
Scrambler therapy is a non-invasive, opioid-sparing treatment for chronic pain.
Recommended Reads:
📘 What is scrambler therapy?
📘 What to Expect During a Scrambler Session
📘 CRPS Pain Relief Without Drugs—Real Patient Stories
📘 Conditions that scrambler therapy can treat
Take the Next Step: Free Consultation at South Florida Scrambler

Every day counts when we suffer from chronic pain. South Florida Scrambler Therapy offers a free initial consultation to determine if Scrambler is right for you. Schedule Today:
- Speak directly with Dr. Rick Markson’s team
- Learn about treatment protocols and insurance
- Complete a customized treatment plan
- Start seeing results within days, not months
📞 Call Now or Visit website: www.southfloridascramblertherapy.com
📍 We serve Palm Beach, Fort Lauderdale, and Miami from our location at 100 NW 100th Ave, Plantation
You Can Follow Us through Our Social Media:
📸Instagram—Day-in-the-life stories from our patients
👍Facebook—Success journeys and community support
You deserve to laugh, and enjoy life without pain. The journey starts here.
Patient Reviews
Start Your Nerve Pain-Free Journey Today







